
Nitin Agrawal
Medical Student
Texas A&M University College of Medicine
Board Member, Longitude.site
Graduating medical students early is not a completely novel concept. During WWII, there was a significant physician shortage, and various medical schools initiated a 3-year accelerated MD program to produce more physicians. These programs were eventually discontinued in the late 1970s and early 1980s. In 1918, the influenza pandemic created a similar situation. Third- and fourth-year medical students were enlisted to help treat the overwhelming number of patients, both those with influenza and those without. Today, COVID-19 resurfaces the question of graduating medical students and other trainees early. Italy, one of the hardest-hit countries, decided to cancel the final exam for its medical students and called upon 10,000 students to help with triage, to perform tests, and to support general practitioners’ clinics.
In the United States, there have been significant discussions of graduating fourth-year medical students early in order to help buffer the front lines. Many medical schools have initiated processes to allow students to voluntarily graduate early, but this is not the nationwide standard. The debate has now centered on whether more schools should and need to do this, especially as different parts of the country face different waves of the pandemic.
Pros
1. Fourth-year medical students can fill the need for providers immediately
By April, most fourth-year medical students have finished their required rotations. Many had vacation or were scheduled to complete online or other electives when the effects of COVID-19 became widespread in the US. For most fourth-year medical students, the amount of new knowledge gained from those electives may not be as critical to their future success. Therefore, fourth-year medical students can fill the need for providers immediately if they are allowed to graduate early. Many fourth-year medical students are currently quarantined at home, and if healthy and able, they can be quickly mobilized to immediately provide relief in critical areas.
2. Fourth-year medical students generally have fewer comorbidities
As COVID-19 continues to drain resources (including able health care personnel), there has been a push to bring retired providers into the front-lines. However, many of our retired providers have comorbidities that put them at a higher risk for more serious complications of COVID-19. While no one is exempt from COVID-19 and its potentially lethal complications, at this point, fewer comorbidities tend to indicate a better prognosis. One could then hypothesize that students with fewer comorbidities are at a lower risk of COVID-19 complications.
3. Fourth-year medical students can help free up more experienced providers
A brand-new intern is not ready to take care of a critically ill patient. However, a brand-new intern can help take care of common “bread and butter” cases (congestive heart failure, COPD, non-COVID-19 pneumonia, etc.). The majority of medical students should have encountered these cases on their internal medicine rotation and other electives. With proper supervision, a new intern can help manage these patients and help free up more experienced providers to treat critically ill COVID-19 patients.
Cons
1. Social distancing would be broken in many cases for fourth-year medical students moving for their residencies
Social distancing is one of the most important weapons to fight the virus. However, by graduating early, potentially tens of thousands of students (and possibly their families) will be required to move to different areas of the country. Additionally, as it is known that COVID-19 can rapidly transmit through asymptomatic carriers, this could lead to the unintentional spread of the virus. This mass movement also puts fourth-year students and their families at risk.
2. Introducing new interns into the front-line would further deplete dwindling PPE [Personal Protective Equipment] resources
PPE is critical in this fight, and unfortunately, we still do not have an adequate supply for all health care providers at risk. While new interns may not directly be the primary doctor for COVID-19 patients, they will undoubtedly need to use PPE for other cases or COVID-19 rule outpatients. While it is absolutely necessary to protect everyone with PPE, an influx of health care providers may put a new strain on an otherwise dwindling precious resource.
3. Fourth-year medical students will be brand new interns and therefore need a lot of oversight
While the July Effect (the idea that teaching hospitals in July have more mistakes/medical errors because new interns start in July every year) has been variably supported and contradicted, it is without a doubt that new interns need close oversight at the beginning of their careers. In a typical environment, upper-level residents provide months of close, individualized oversight until interns are able to take on more and more responsibility. However, additional oversight will reduce the overall time upper-level residents have while they continue to juggle complex patients, including COVID-19 cases.
A fourth-year’s perspective
As a fourth-year medical student, I can see both perspectives and do not know the right answer. A big part of me wants to help and be part of the front-lines. I went to medical school to ultimately provide care, and there is no better time than the present. However, a part of me understands that there are more complex issues at hand. Could I be doing more harm than good by rushing into residency? Would my presence create an extra burden? In this time of great uncertainty, these decisions cannot be taken lightly. However, due to the evolving nature of the pandemic, it is critical that medical schools nationwide discuss this internally as well as with their local hospitals, academic institutions, governing bodies, and the CDC in order to be ready when a decision must be made. As COVID-19 permeates the country, the need for health care workers on the front-line becomes ever more pressing. Should fourth-year medical students fill that void?
Article originally published on KevinMD.
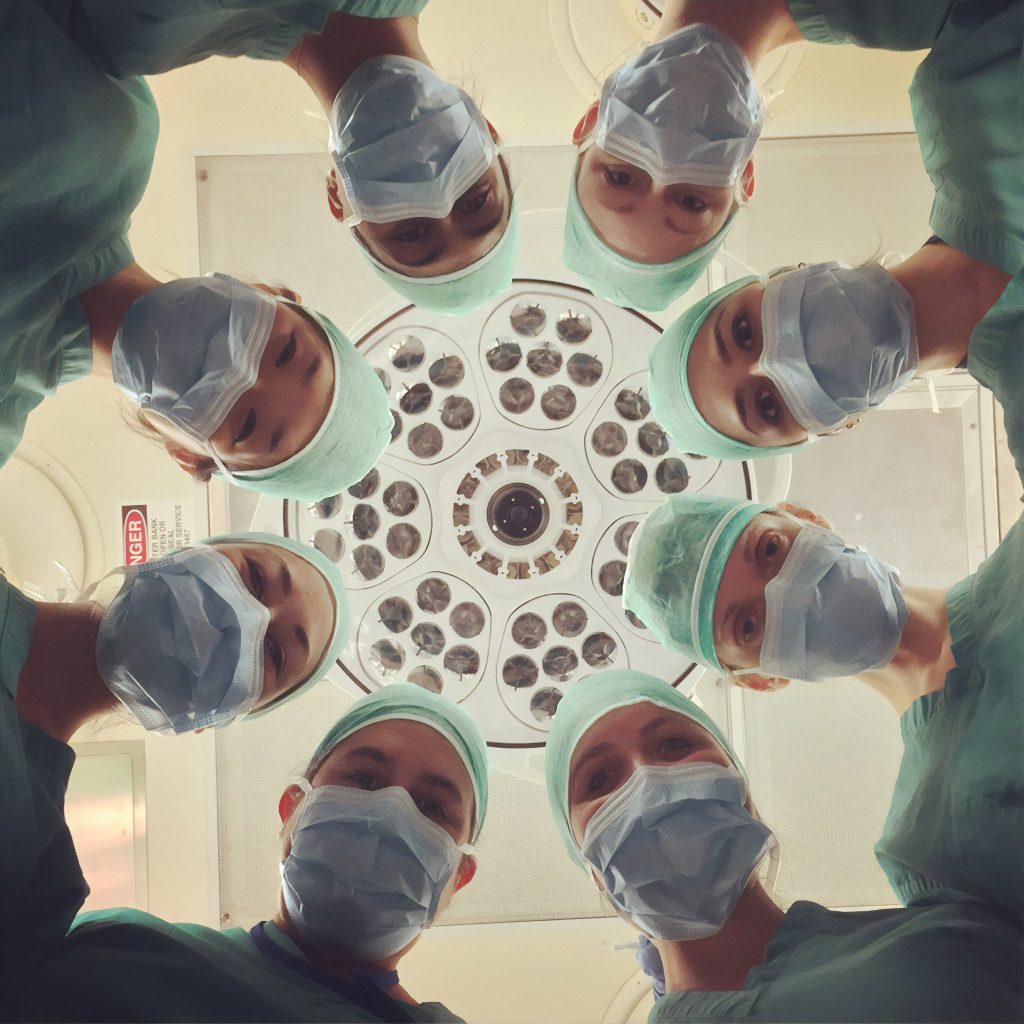
Photo by National Cancer Institute on Unsplash
